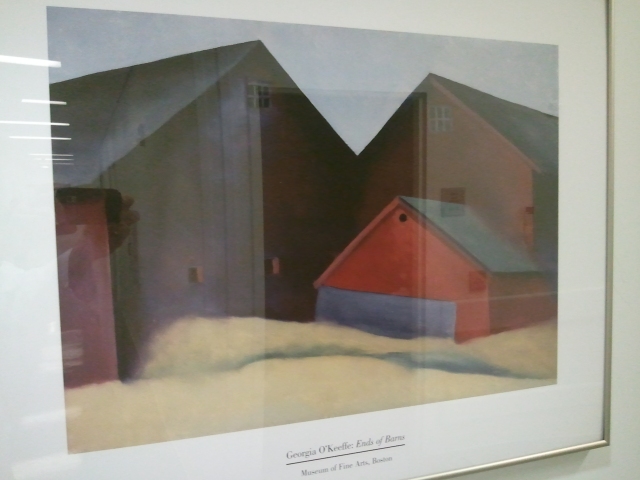
A favorite Georgia O'Keefe - "Ends of Barns"
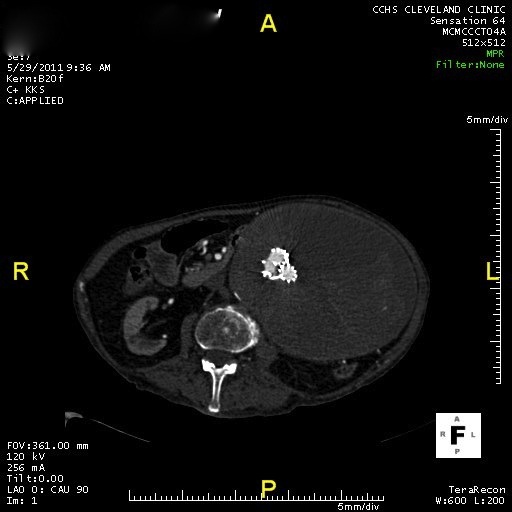
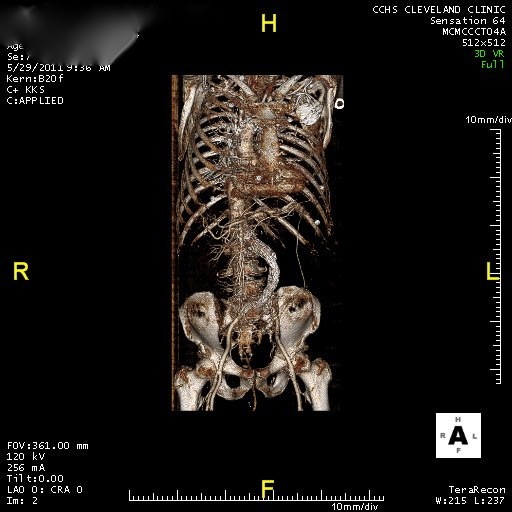
Well our lysis from Thursday (the marathon man) had some re-thrombosis through the night as a result of the on call fellow stopping the TPA because of a very low fibrinogen level. But this provided a valuable lesson for me. Not only was the discontinuation of the TPA a questionable move but the management changed and we took an aternative mechanical thrombolytic route. The Trellis Catheter® allowed us to isolate the affected areas, bolus more TPA into the isolated area and mechanically macerate and aspirate the clot. In combination with the Angio-Jet pulse aspirator we cleared essentially all of his clot burden and uncovered his Iliac vein compression (May-Thurner’s syndrome). This was successfully stented. He was started on Lovenox post procedure and hopefully will go home soon.
Our second case was a continuing lysis of an aorto bifem bypass graft. He had some residual clot at the right femoral anastomosis which was treated by a Craig-McNamara catheter infusing TPA overnight. This morning he had some residual “stuff” at the anastomosis of his graft to the femoral artery. This may represent old clot or scar tissue. We ballooned the area and saw some improvement but decided it will best be managed by open endarterectomy / patch. We were able to place a 8 mm balloon expandable stent at the aorta / graft anastomosis and then post dilate to 12 mm via his 6 french brachial sheath. This looks to be an excellent result for this unfortunate gentleman.
On second call today. Made rounds on the MEGA service (acronym for the attending staff names) ICU patients. Besides the tuition payment we made for this experience the on call assignment is the cost of this education. Ravi, our second year Fellow in charge of the call calendar, is very understanding and accommodating when making my assignments. He is trying to keep me off the weekday call but this means weekends are tied up here in Cleveland. This weekend we are enjoying lovely thunderstorms. In addition, they are conducting “Spring cleaning” in the 89th street parking deck which means I had to find another place to park at 5:45 this AM. Fortunately things do quiet down a lot on weekends so there were plenty of options.
I continue to marvel at the array of patients that are cared for here at CC. One patient on the service is a homeless psychotic man who had an ax fem bypass to (hopefully) allow him to heal an above knee amputation. Last night a Kuwaiti gentleman arrived with an abdominal aneurysm and chronic abdominal pain. He also has TB. There are many patients from the Cleveland area but just as many from the wide radius of northwest Ohio. A steady cohort of patients hails from the remaining lower 48. As a consequence of their reputation, CC receives many prominent “well connected” individuals. I often hear the discussion about “special treatment” wind up with “treat ’em just like the last one.” Making exceptions for individuals seems to be the quickest route to errors and complications. This was scrupulously avoided recently with a patient on our vascular service. He was succinctly described as a “friend of Toby” as in Delos “Toby” Cosgrove, MD, the CEO of the Cleveland Clinic. This patient is widely connected to executives around the country and the world. Through his network he funnels approximately a thousand families to the Cleveland Clinic each year. Needless to say this group of patients creates a sizable stream of donations to the Cleveland Clinic Foundation. While our patient had the constant attention of one of the staff cardiac anesthesiologists (a personal friend of his) during his vascular procedures, everyone consciously tried to treat him the “same as the last one“.
Despite their outstanding well deserved reputation as an international medical and surgical destination, the Cleveland Clinic struggles with many of the same issues that every hospital faces. Among the sea of outstanding medical personnel there are a handful of individuals who “stand out” for their less than stellar qualities. A vascular surgeon who had such difficulty respecting the fellows and residents that he was removed from the teaching service, the nurse anesthetist who is so “loopy” that staff warn me to question every drug and dose she gives “just to be sure”, the radiology tech who can’t remember the button sequence for activating the Angio-Jet (after two years) and the Vascular Fellow who plods along as the department “sad-sack” raising the ire of attendings, fellows and residents on a regular basis. These people are the sand in the gears that remind me of Jay Fisher’s favorite quote (one of many) – “Never confuse success with continuing to be successful.” It takes a constant commitment to excellence to occasionally achieve success. Continuing to find the right people and placing them in the right roles and positions is the greatest challenge of leadership and is far more important than any policy, protocol or mission statement in building excellence. At the same time, reassigning, removing or weeding out the bottom 10% of employees can shackle the most deft managers requiring their relentless attention. Discriminating excellence from success was nicely examined by Joe Paterno in an address to Sports Medicine physicians in 1990.
There are many people, particularly in sports, who think that success and excellence are the same thing and they are not the same things. Excellence is something that is lasting and dependable and largely within a person’s control. In contrast, success is perishable and is often outside our control. If you strive for excellence, you will probably be successful eventually. People who put excellence in first place have the patience to end up with success. An additional burden for the victim of the success mentality is that he/she is threatened by the success of others and resents real excellence. In contrast, the person fascinated by quality is excited when he/she sees it in others.
Yes, that was Joe Paterno. I think we need to guard against the success mentality in our health care institutions and encourage our leadership and administration to build on excellence. While money can follow success, REAL money follows excellence.

Somedays I would like to be hiking in Colorado